Chronic Pediatric Pancreatitis and (No) Persistent Belly Pain
Chronic Pediatric Pancreatitis and (No) Persistent Belly Pain https://pediatricsnationwide.org/wp-content/uploads/2021/03/AdobeStock_82850633_header-1024x575.jpg 1024 575 Katie Brind'Amour, PhD, MS, CHES Katie Brind'Amour, PhD, MS, CHES https://pediatricsnationwide.org/wp-content/uploads/2021/03/Katie-B-portrait.gif- July 05, 2021
- Katie Brind'Amour, PhD, MS, CHES

Underlying — even silent — chronic pancreatitis can be at play in children without previous acute pancreatitis episodes, including among children with little or no reported pain.
Pancreatitis in children is rare (about 3-13 per 100,000 people per year), but diagnosis is increasing, at least in part due to increased awareness among physicians. The path to diagnosis, however—even for children with acute and recurrent episodes of pancreatitis — is not always straightforward; many patients report suffering with stomach problems for years prior to being diagnosed. Repeated episodes of acute pancreatitis in children can cause damage to accumulate, leaving them more likely to develop chronic pancreatitis.
Indeed, when INSPPIRE (INternational Study group of Pediatric Pancreatitis: In search for a cuRE) investigators examined their database to separate chronic pancreatitis patients into subgroups by diagnostic history, they uncovered surprising data.
“We found a group of children diagnosed with chronic pancreatitis who had no history of acute pancreatitis,” says Cheryl Gariepy, MD, a pediatric gastroenterologist and director of the Pancreas Center at Nationwide Children’s Hospital. The specialty center is designated as a National Pancreas Foundation Center of Excellence. Dr. Gariepy is also one of the original members of the INSPPIRE team. “There are patients who already have these permanent changes when they are first evaluated, suggesting that something’s been brewing for some time, but they have never had a recognized episode of acute pancreatitis.”
Their findings were published in Pancreatology, reporting that as many as 10% of children diagnosed with chronic pancreatitis had no prior diagnosis of acute or acute recurrent pancreatitis, which they termed “silent” chronic pancreatitis. Children with silent chronic pancreatitis were more likely to have autoimmune pancreatitis and ductal stones (an advanced morphological change) than children diagnosed with chronic pancreatitis after episodes of confirmed acute pancreatitis.
A 2016 INSPPIRE publication in JAMA Pediatrics also revealed that as many as 28% of children with chronic pancreatitis report either no abdominal pain or say that they are usually pain free, with episodes of mild-to-moderate pain, while 41% had constant mild-to-moderate pain (with or without episodes of severe pain) or constant severe pain.
“It may be that children with silent chronic pancreatitis had pain episodes not recognized as pancreatitis, or that they experienced pancreatic damage through mechanisms that don’t produce severe pain and acute pancreatitis,” says Dr. Gariepy, who is also a professor of pediatrics at The Ohio State University. “INSPPIRE research has shown us that not all pancreatic damage causes pain, which is why pain is specifically not a criterion to diagnosed chronic pancreatitis in children.”
Chronic pain is a key symptom to trigger evaluation for chronic pancreatitis in adults. But in children, there is no requirement for pain — just permanent damage detected on imaging, plus pain and/or loss of function.
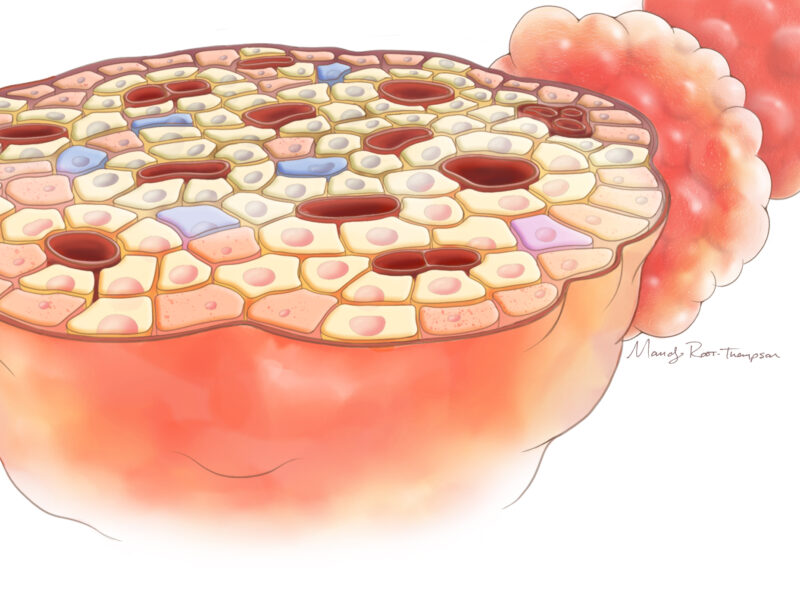
In the past decade, researchers have significantly advanced the understanding of the mechanisms of acute pancreatitis, including the regulators of acinar cell injury, ductal function and trypsin activation. Recent studies in chronic pancreatitis indicate that there is more than one pattern of pancreatic tissue destruction, which may vary in their ability to trigger acute pancreatitis. Cystic fibrosis, for example, produces fatty replacement of pancreatic tissue, while SPINK1 mutations, autoimmune pancreatitis and alcohol abuse lead to pancreatic fibrosis.
“We are just learning about ways the pancreas can be severely damaged without triggering acute pancreatitis,” says Dr. Gariepy.
In an effort to identify the mechanisms and the genes or gene combinations at play behind this subpopulation of chronic cases, INSPPIRE is running genetic testing on more than 300 children with pancreatitis. Dr. Gariepy and her INSPPIRE colleagues also recently reported on the impact of pain on quality of life in children with pancreatic disease at a national meeting.
“The main lesson from this is to consider pancreatitis in your patients having belly pain, even if it is just mild pain,” says Dr. Gariepy. “There are a lot of causes of belly pain, and it’s a small fraction of children that have pancreatitis, but it is still important to consider that diagnosis, send a lipase test, and think about imaging for those patients.”
Considering pancreatitis more often may help catch more so-called “silent” chronic pancreatitis patients, or catch some kids earlier with acute forms of the condition. And if a single acute pancreatitis episode is confirmed, she adds, clinicians should be on the lookout for recurring pancreatitis.
“Up to 30% of children with pancreatitis will have it recur,” says Dr. Gariepy. “And if it recurs, those children should be referred to a pancreatitis specialty center.”
References:
- Abu-El-Haija M, Lowe M, Barth B, Bellin MD, Fishman DS, Freedman S, Gariepy C, Giefer MJ, Gonska T, Heyman MB, Himes R, Husain S, Lin TK, Liu Q, Mascarenhas MR, Maqbool A, McFerron B, Morinville V, Nathan J, Ooi CY, Perito E, Pohl JF, Schwarzenberg SJ, Shah U, Troendle D, Werlin S, Wilschanski M, Zimmerman B, Uc A. Pediatric chronic pancreatitis without prior acute or acute recurrent pancreatitis: A report from the INSPPIRE consortium. Pancreatology. 2020 Jun;20(4):781-784.
- Kumar S, Ooi CY, Werlin S, Abu-El-Haija M, Barth B, Bellin MD, Durie PR, Fishman DS, Freedman SD, Gariepy C, Giefer MJ, Gonska T, Heyman MB, Himes R, Husain SZ, Lin TK, Lowe ME, Morinville V, Palermo JJ, Pohl JF, Schwarzenberg SJ, Troendle D, Wilschanski M, Zimmerman MB, Uc A. Risk Factors Associated With Pediatric Acute Recurrent and Chronic Pancreatitis: Lessons From INSPPIRE. JAMA Pediatrics. 2016 Jun 1;170(6):562-9.
- Tham S, Cress G, Yuan Y, et al. Su1505. Health-related quality of life, emotional, and behavioral functioning in children with acute recurrent or chronic pancreatitis. Gastroenterology. 2020;158:S-607.10.1016/S0016-5085(20)32219-8.
Image credit: Adobe Stock
About the author
Katherine (Katie) Brind’Amour is a freelance medical and health science writer based in Pennsylvania. She has written about nearly every therapeutic area for patients, doctors and the general public. Dr. Brind’Amour specializes in health literacy and patient education. She completed her BS and MS degrees in Biology at Arizona State University and her PhD in Health Services Management and Policy at The Ohio State University. She is a Certified Health Education Specialist and is interested in health promotion via health programs and the communication of medical information.
-
Katie Brind'Amour, PhD, MS, CHEShttps://pediatricsnationwide.org/author/katie-brindamour-phd-ms-ches/April 27, 2014
-
Katie Brind'Amour, PhD, MS, CHEShttps://pediatricsnationwide.org/author/katie-brindamour-phd-ms-ches/April 27, 2014
-
Katie Brind'Amour, PhD, MS, CHEShttps://pediatricsnationwide.org/author/katie-brindamour-phd-ms-ches/April 27, 2014
-
Katie Brind'Amour, PhD, MS, CHEShttps://pediatricsnationwide.org/author/katie-brindamour-phd-ms-ches/April 28, 2014
- Post Tags:
- Gastroenterology and Hepatology
- Pancreas