Choking Education an Important Element of Care for Prader-Willi Syndrome Families
Choking Education an Important Element of Care for Prader-Willi Syndrome Families https://pediatricsnationwide.org/wp-content/uploads/2020/07/PWS5.jpg_header-1024x575.jpg 1024 575 Katie Brind'Amour, PhD, MS, CHES Katie Brind'Amour, PhD, MS, CHES https://pediatricsnationwide.org/wp-content/uploads/2021/03/Katie-B-portrait.gif- July 31, 2020
- Katie Brind'Amour, PhD, MS, CHES

Choking prevention and intervention education offer a simple way to address this common cause of death among PWS patients.
Individuals with Prader-Willi Syndrome (PWS) suffer from poor oral muscle control, generalized low muscle tone that can make it hard to swallow properly, a poor gag reflex and an insatiable desire to eat. Together with a low production of saliva and a tendency to rush food consumption (not chewing properly, consuming large quantities or sneaking food quickly), patients can be uniquely predisposed to suffer from a choking incident — and, indeed, to die from one.
Choking is common in this population, affecting at least 1 in 3 patients during their lifetimes, and leading to death in about 8% of the PWS population, according to research in the American Journal of Medical Genetics published in 2007. Furthermore, the risk is not restricted to very young children, with the average age of death due to choking at about age 24. It appears to predominantly occur in males.
When Amy Moffett, CPNP-PC, a nurse practitioner in the Prader-Willi Syndrome Clinic at Nationwide Children’s, learned of the prevalence of this problem at the Pediatric Endocrinology Nursing Society (PENS) Conference in 2017, she knew it offered an opportunity to change the quality — and perhaps even the duration — of life for the clinic’s PWS patients.
“It was clear that we needed to offer our families choking-related education and some first aid training,” says Moffett. “Obviously, our goal is that nobody chokes, but if something does happen, we want families to know what to do.”
Moffett and her colleague Kathryn Anglin, RN, MSN, a long-time nurse in the PWS Clinic at Nationwide Children’s, worked with clinic endocrinologists, nursing staff and community programming teams at the hospital to develop a basic choking education and prevention training for families. Families were given a pre- and post-test to assess their knowledge about choking risks and their comfort level with choking interventions. Based on pre-test data, about 1 in 3 families reported that their child had experienced a choking episode and, of those, about half had required intervention.
All of the education was delivered during waiting periods between visits with different clinicians in the multidisciplinary clinic. Families watched an age-specific choking prevention and intervention video developed by the American Heart Association. They also had the chance to practice the Heimlich maneuver on mannequins. Although it did not involve a formal first aid certification, families received information on where they could pursue further CPR training locally.
Families also received a choking education packet that included both PWS-specific and generic choking information, enabling the team to emphasize the importance of food security practices such as designating a “food watcher” during holiday events and changes in routine, avoiding high-risk foods, cutting all foods into small pieces, locking cupboards and fridges, sharing the information with schools and care assistants and more.
“It is something we don’t think about as endocrinologists very often because it’s not part of the endocrine system, but an increased risk of choking is something we need to think about within our patients’ full spectrum of disease,” says Kathryn Obrynba, MD, director of the PWS Clinic at Nationwide Children’s. “I can’t say enough how simple it was for us to integrate this education into our clinical workflow.”
Within 12 months of initiating the QI project, the team surpassed their goal of educating 80% of the clinic’s PWS families. The project has also demonstrated clear post-test improvements in family knowledge of choking risks and comfort with interventions.
The team plans to start asking families about choking history at each visit, to better document incidence and trigger related education as needed. They also plan to maintain the education program as a routine part of clinical practice moving forward and will publish their findings.
“We believe in the simplicity and importance of this training so much that it has become a permanent and widespread change in practice for us,” says Moffett, who presented the team’s QI results at the PENS Conference in 2019. “It should be part of family education in every PWS clinic.”
References:
- Manzardo AM, Loker J, Heinemann J, Loker C, Butler MG. Survival trends from the Prader-Willi Syndrome Association (USA) 40-year mortality survey. Genetic Medicine. 2018;20(1):24-30.
- Moffett A, Anglin K. Prader-Willi Syndrome choking prevention and education: A practice change. Presentation at the Pediatric Endocrinology Nursing Society: Long Beach, CA. April 27, 2019.
- Stevenson DA, Heinemann J, Angulo M, et al. Deaths due to choking in Prader-Willi syndrome. American Journal of Medical Genetics A. 2007;143A(5):484-487.
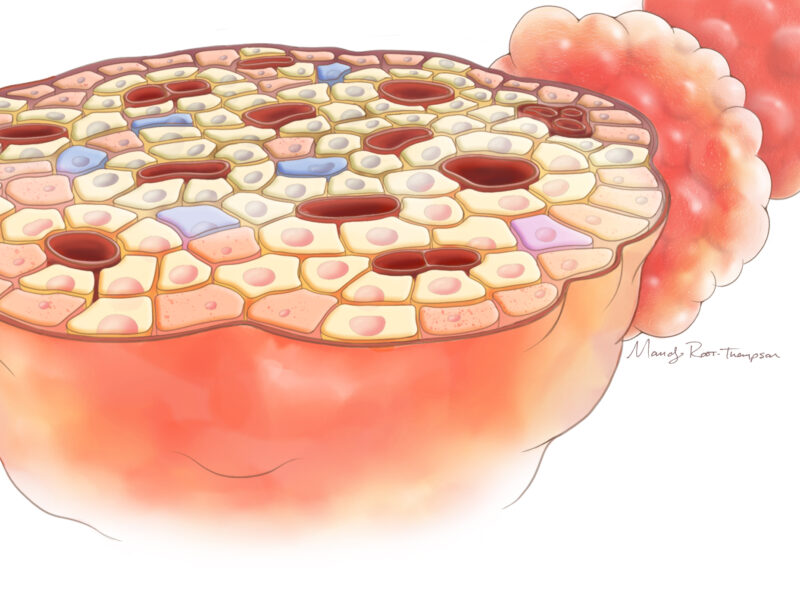
Image credit: Nationwide Children’s
About the author
Katherine (Katie) Brind’Amour is a freelance medical and health science writer based in Pennsylvania. She has written about nearly every therapeutic area for patients, doctors and the general public. Dr. Brind’Amour specializes in health literacy and patient education. She completed her BS and MS degrees in Biology at Arizona State University and her PhD in Health Services Management and Policy at The Ohio State University. She is a Certified Health Education Specialist and is interested in health promotion via health programs and the communication of medical information.
-
Katie Brind'Amour, PhD, MS, CHEShttps://pediatricsnationwide.org/author/katie-brindamour-phd-ms-ches/April 27, 2014
-
Katie Brind'Amour, PhD, MS, CHEShttps://pediatricsnationwide.org/author/katie-brindamour-phd-ms-ches/April 27, 2014
-
Katie Brind'Amour, PhD, MS, CHEShttps://pediatricsnationwide.org/author/katie-brindamour-phd-ms-ches/April 27, 2014
-
Katie Brind'Amour, PhD, MS, CHEShttps://pediatricsnationwide.org/author/katie-brindamour-phd-ms-ches/April 28, 2014
- Posted In:
- Clinical Updates
- In Brief