Bouncing Back: Overcoming Physician Burnout With Resilience
Bouncing Back: Overcoming Physician Burnout With Resilience https://pediatricsnationwide.org/wp-content/uploads/2017/09/080417BS0072_Smaller-Mahan_Reed-header-1024x575.gif 1024 575 Suzanne Reed, MD and John Mahan, MD Suzanne Reed, MD and John Mahan, MD https://pediatricsnationwide.org/wp-content/uploads/2021/03/Suzanne-Reed.gif- September 12, 2017
- Suzanne Reed, MD and John Mahan, MD

Physician burnout is becoming increasingly recognized as an extensive and debilitating reality. Present in specialties across the spectrum of medicine, most disciplines report burnout rates of 50 to 60 percent or more, and these rates have been increasing over the last several years. Pediatrics alone demonstrated a more than 16 percent increase in burnout, up from 35 percent in 2011 for general pediatricians. Burnout has been defined as a “state of mental and physical exhaustion related to work or care-giving activities.” The Maslach Burnout Inventory, the reference standard for measuring burnout, utilizes three domains in describing and characterizing burnout: high emotional exhaustion, high depersonalization and low sense of personal accomplishment.
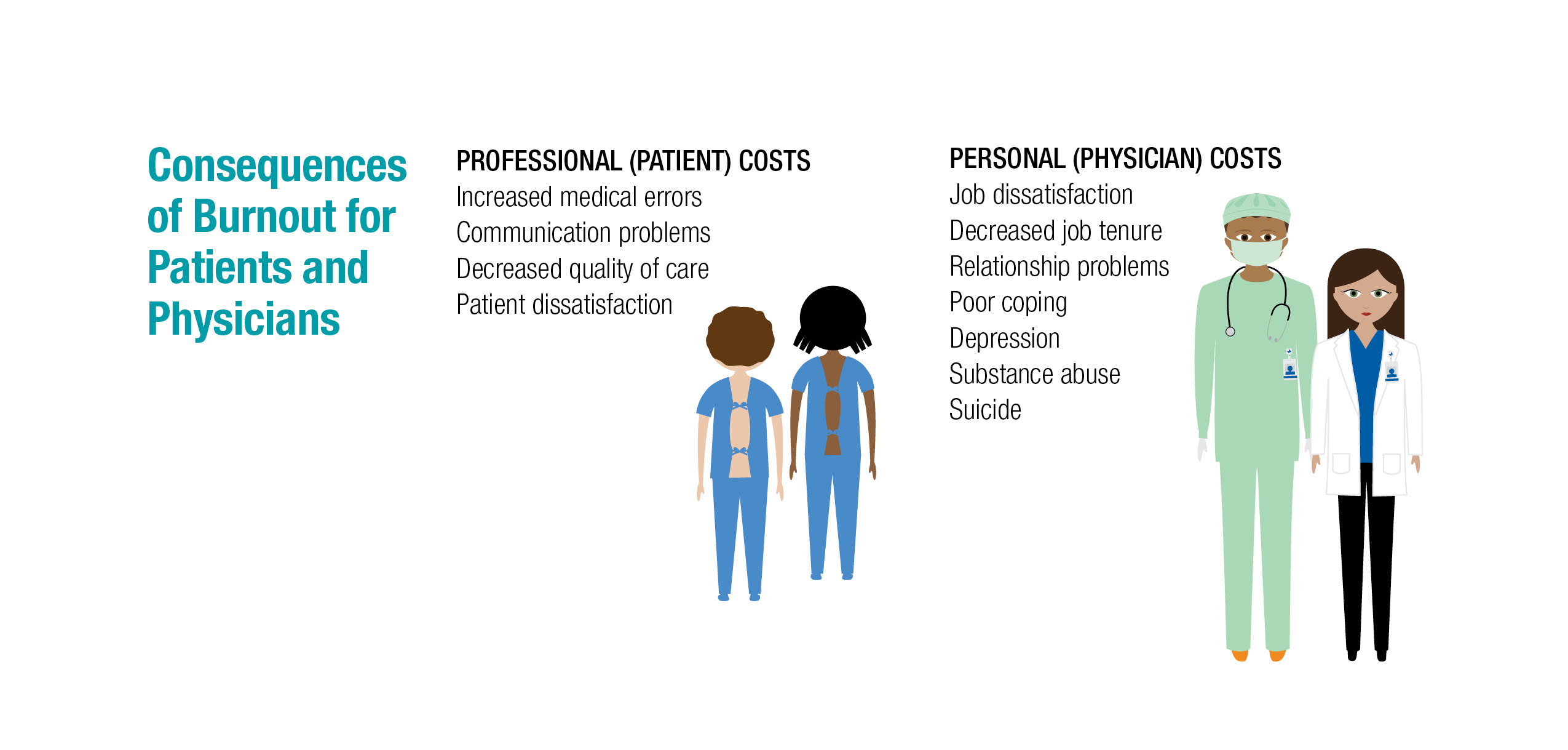
The consequences of burnout are significant, from professional consequences such as poorer patient outcomes; for example, increased medical errors and lower quality of care; to personal problems such as inability to cope, leading to increased rates of substance abuse and death by suicide.
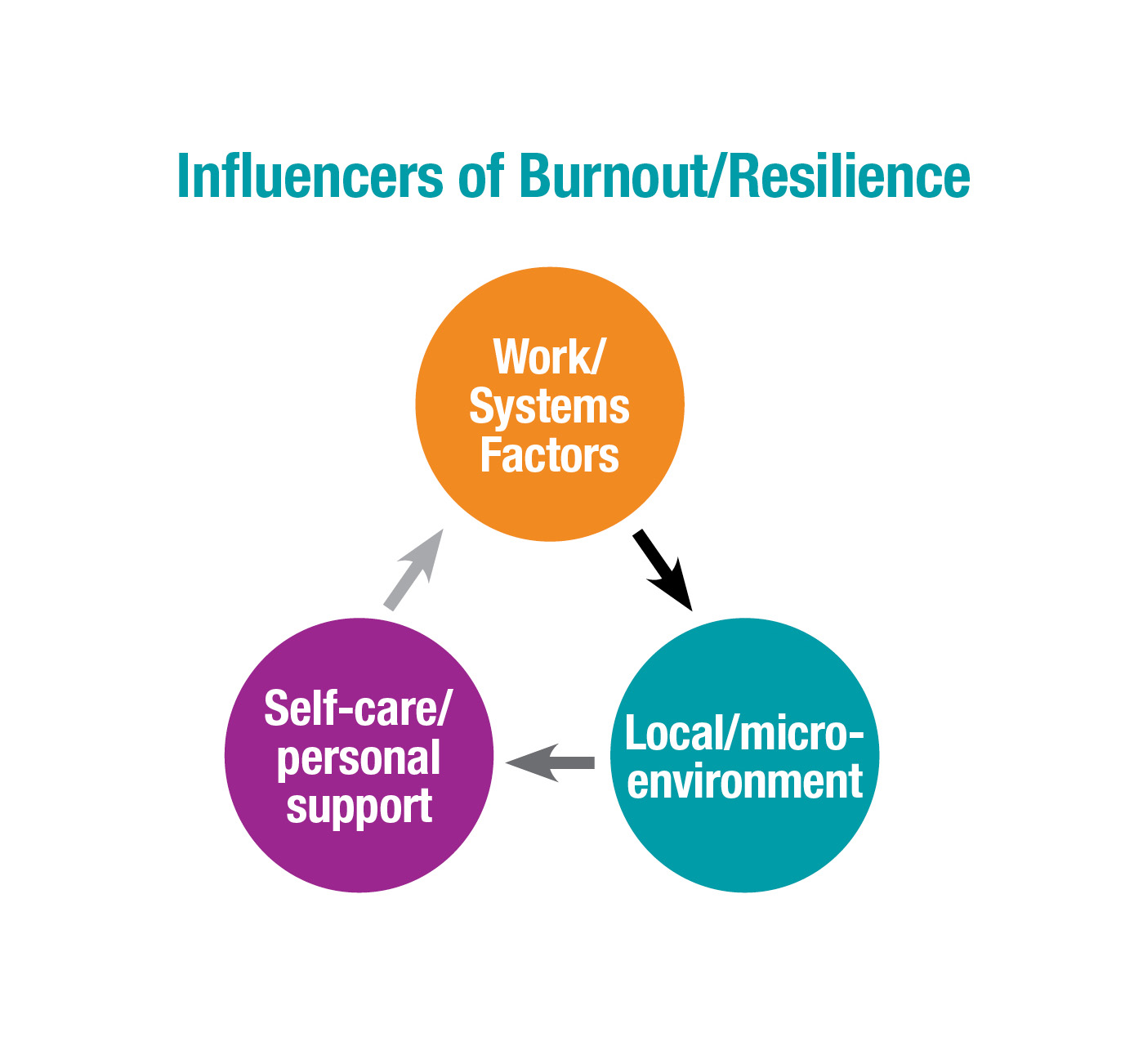
Causes of burnout fall into three main categories: systems issues, such as bureaucratic overload; divisional/local issues, such as difficult patients; and personal issues, such as family stressors and lack of self-compassion and self-care. Burnout is more prevalent in female physicians across subspecialties, and they report less happiness at work than male physicians, as well.
Resilience is the ability of an individual to respond to stress in a healthy, adaptive way so that personal goals are achieved at reasonable psychological and physical costs, and we believe it is the primary protection against burnout. The nature of medicine is to care for vulnerable individuals and cope with illness and undesired outcomes; resilience allows physicians to withstand and “bounce back” from the challenges associated with these duties.
As physician-educators, we endorse multiple complementary methods to promote resilience, such as (1) attending to self-awareness, self-care, optimism, gratitude, mind-body skills and (2) pursuing enhanced support and community-building for physicians. Mitigating burnout is best addressed through a multifaceted professional and personal approach. Professionally, we must prioritize balancing excessive workload and improving efficiency for physicians in their clinical work. Promoting physician autonomy by valuing input and facilitating engagement can be very powerful. Personally, encouraging efforts at work-life balance, or rather work-life integration, can foster the healthy proportion of work and life and acknowledge the interconnectedness of our relationships, roles and responsibilities in all facets of our lives. Balance implies competition between the elements of work and life, or at least their independent existences. In today’s technological age, the boundaries of our work and lives increasingly overlap, and healthy work-life integration is a more realistic and useful goal.
An essential facet of healthy work-life integration is uncovering, re-establishing and maintaining the intrinsic and extrinsic meaning in our work. It is that which, for most of us, compelled us to become physicians, and that which defines our work as not simply a job, but a calling.
Institutions must work to improve and optimize work environments to promote institutional physician resilience. On a local level, leaders can develop more effective team functions to better support physicians and other team members. Focused rewards and recognition of accomplishments can promote a cohesive, supportive local environment and foster resilience.
It is important to recognize that work on systems and local environments are only part of the path to resilience. Personal growth and development are arguably as important and certainly under the control of the individual physician. Mindfulness and meditation have been shown to enhance resilience in physicians. Purposeful focus on gratitude, such as keeping a gratitude journal, and maintaining a healthy perspective are other routines associated with wellness. Positive thinking is another life practice that fosters resilience; it describes the ability to experience both negative and positive emotions in difficult situations and the capacity to find redeeming value in the challenges. Notably, these are all skills that can be learned by anyone with proper instruction and, most importantly, deliberate practice. Additionally, adequate sleep, exercise and a healthy diet are so basic (and so often neglected), yet so essential to personal wellness and enhanced resilience.
It is insufficient to only understand and acknowledge burnout. Cultivating true resilience in physicians through system changes and promoting wellness and self-care is the path beyond burnout. It will require a concerted and integrated effort between systems, leadership and individual physicians to create and enforce a culture which develops and values resilience. This requires a paradigm shift for the medical profession and necessitates the letting go of long-held professional norms that have implicitly expected physicians to simply work on, work harder, and endure. Resiliency allows physicians to flourish while staying connected with their own missions, values and priorities at work and in life. The stakes and rewards for our patients and our society will be profound.
Ready to join the conversation? Follow Dr. Mahan on Twitter @MedEdMahan.
Image credits: Nationwide Children’s
About the author
Dr. Reed's clinical interests focus on pediatric leukemia. She has a research interest in medical education, specifically in the teaching of communication and breaking bad news skills. Dr. Reed has a programmatic interest in medical education. She is developing a communication curriculum for the pediatric residency program, for which she serves as an associate program director. Dr. Reed received her medical degree from The Ohio State University College of Medicine. She completed both her residency and fellowship at Nationwide Children's.
-
John Mahan, MDhttps://pediatricsnationwide.org/author/john-mahan-md/September 12, 2017
- Posted In:
- Features