Uncovering Why Synthetic Tracheal Replacements Fail, and Hints for Success
Uncovering Why Synthetic Tracheal Replacements Fail, and Hints for Success https://pediatricsnationwide.org/wp-content/uploads/2020/04/AdobeStock_238705659-header-1024x575.jpg 1024 575 Kevin Mayhood Kevin Mayhood https://secure.gravatar.com/avatar/bd57a8b155725b653da0c499ae1bf402?s=96&d=mm&r=g- April 10, 2020
- Kevin Mayhood
“There is no ideal replacement for the trachea,” says Tendy Chiang, MD, a pediatric otolaryngologist and a principal investigator in the Center for Regenerative Medicine in the Abigail Wexner Research Institute (AWRI) at Nationwide Children’s Hospital.
“There are many surgical techniques that can manage tracheal defects and disorders, however, for longer-segment defects, they oftentimes require replacement tissue that just isn’t available,” says Dr. Chiang, who is also an assistant professor in the Department of Otolaryngology – Head and Neck Surgery at The Ohio State University College of Medicine. “There’s no autologous substitute.”
Tissue-engineered tracheal grafts (TETGs) were thought to be a promising solution, but clinical trials in Europe were halted due to failures.
In the wake of the troubles, Dr. Chiang and colleagues, who were not involved in the European trials, have undertaken systematic investigations into why the implants fail and possible solutions.
“What happened in Europe is they went too fast,” says Susan Reynolds, PhD, a principal investigator in the Center for Perinatal Research in AWRI at Nationwide Children’s working with Dr. Chiang. Dr. Reynolds’ efforts focus on tissue stem cells that maintain the conducting airway epithelium. “We definitely know what the endgame is but solving the problem is going to take many steps.”
Bit by bit, the research team has produced three sets of data.
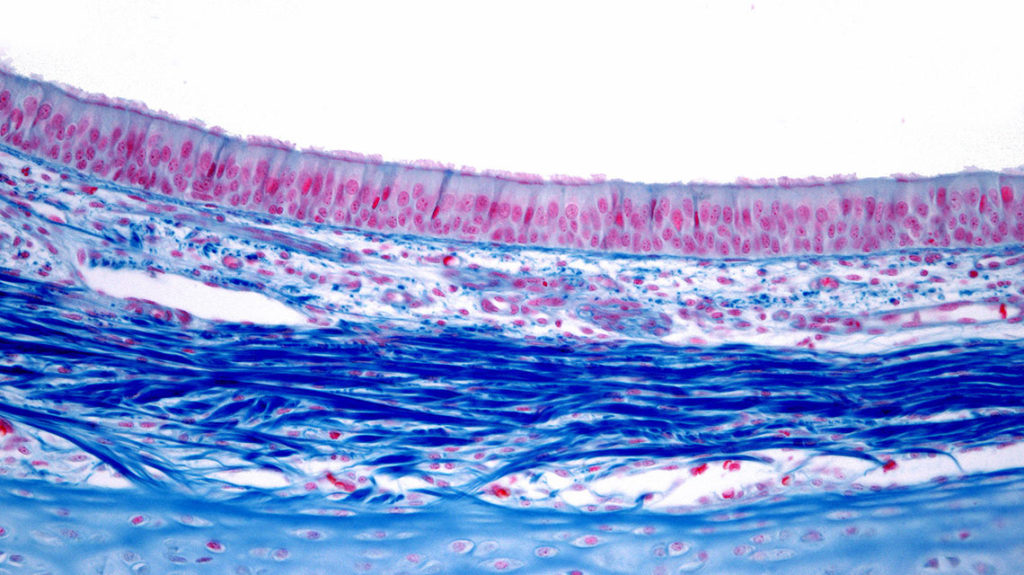
“In vitro data shows that the progenitor cell population is adversely affected by the scaffold,” Dr. Chiang says. “Large animal data show the synthetic implants don’t re-epithelialize well. And, data from a small animal model show that at the right scale, the implant does restore the epithelium and a functional one at that.”
In their large animal study, the researchers implanted the same type of TETGs and replicated the processes used in the trials abroad. The long-term outcomes were similarly poor. Grafts narrowed, infections occurred where synthetic and native trachea joined and no epithelialization or neovascularization occurred.
To try to understand why epithelialization did not occur, Dr. Reynolds led the effort to determine whether airway epithelial stem cells could attach to the porous scaffold and if they could attach, could they grow? Then, if the answers were “yes,” could the stem cells make a functional epithelium?
Her team made in vitro comparisons of electrospun polyethylene terephthalate and polyurethane (PET/ PU) TETGs, like those used in the European trials, and a polystyrene control scaffold. The control lacks the biomechanical properties needed for an implant, but the cells are known to grow well on its surface.
They found native tissue-derived epithelial cells migrated poorly on the PET/PU material compared to control material and that the PET/PU scaffold failed to support basal stem/progenitor cell proliferation.
“We think the stem cells are not able to interact or attach to the PET/PU scaffold, so like grains of sand they’re just filtering through and finally getting down to the polystyrene base, and that’s a surface the stem cells can attach to,” says Dr. Reynolds, who is also an assistant professor at Ohio State. “If they grow at all, what they do is just make a column of cells.”
“It needs to be a layer and function as a barrier,” she adds.
Surprisingly, when Dr. Chiang tested a PET/PU scaffold patch on small defects in mouse models, the patch re-epithelialized quickly, he says — in two weeks.
“Not only did histology indicate the patch implant formed what appeared to be an epithelium but immunofluorescence revealed this was functional tissue,” Dr. Chiang says.
To narrow the reasons longer-segment implants may fail, the team tested whether morbidity of tracheal replacement in and of itself is contributing to failure. Avoiding detrimental immune responses, the investigators implanted genetically-identical tracheas from one mouse into another, just connecting ends of the donor trachea with the host’s.
“The grafts heal remarkably well and do not develop stenosis or collapse or show signs of respiratory distress,” Dr. Chiang says.
Because of the natural lack of blood supply to the trachea, other studies have suggested a need for staging TETG implants by first putting them where they can create a new blood supply and then implanting them in the windpipe. But the success of the syngeneic implants suggests that with the right construct, that may not be necessary, the researchers say.
Whether or not graft seeding helps with performance of the implants has been controversial. In the mouse models, the investigators saw no differences in the degree of epithelialization or the model’s survival when using grafts seeded with bone marrow mononuclear cells versus unseeded.
The investigators found, however, that seeded cells are rapidly cleared from the scaffold. They suggest that strategies to improve the persistence of seeded cells potentially could influence the outcome, but that remains to be seen.
The researchers are continuing their investigations, Dr. Chiang says. “The next questions are how can we accelerate the re-epithelialization process and how can we incorporate and improve compatibility of these materials with the body so that we can scale up from a patch model to something more clinically viable.”
References:
- Schwartz CM, Stack J, Hill CL, Lallier SW, Chiang T, Johnson J, Reynolds SD. Electrospun scaffolds limit the regenerative potential of the airway epithelium. Laryngoscope Investigative Otolaryngology. 2019 Aug; 4(4):446-454.
- Dharmadhikari S, Liu L, Shontz K, Wiet M, White A, Goins A, Akula H, Johnson J, Reynolds SD, Breuer CK, Chiang T. Deconstructing tissue engineered trachea: Assessing he ole of synthetic scaffolds, segmental replacement and sell seeding on cell performance. Acta Biomaterialia. 2020 Jan 15;102:181-191.
- Pepper V, Best CA, Buckley K, Schwartz C, Onwuka E, King N, White A, Dharmadhikari S, Reynolds SD, Johnson J, Grischkan J, Breuer CK, Chiang T. Factors influencing poor outcomes in synthetic tissue-engineered tracheal replacement. Otolaryngology – Head and Neck Surgery. 2019 Sep;161(3):458-467.
Image credit: Adobe Stock
About the author
-
Kevin Mayhoodhttps://pediatricsnationwide.org/author/kevin-mayhood/
-
Kevin Mayhoodhttps://pediatricsnationwide.org/author/kevin-mayhood/April 25, 2015
-
Kevin Mayhoodhttps://pediatricsnationwide.org/author/kevin-mayhood/April 25, 2015
-
Kevin Mayhoodhttps://pediatricsnationwide.org/author/kevin-mayhood/April 25, 2015
- Posted In:
- Features







